Heaped commissions allow brokers to receive a large commission upfront, up to 75%. This structure has misaligned the business model for voluntary (supplemental) benefits.
Key Takeaways:
- Heaped commissions were born decades ago when the high costs associated with voluntary benefits, like on-site enrollers, were offset by high first-year commissions
- The heaped business model still permeates the voluntary benefits industry because brokers are incentivized by higher income but need to change carriers every few years to receive another round of heaped commission
- This causes high first-year losses for carriers and persistent disruption for employees
- Employer awareness and more transparency in HR benefits administration are finally becoming more common
Commission structures for voluntary benefits continue to be an issue for the insurance industry. The problem stems particularly from heaped commissions, where brokers are compensated a very high percentage in year one. This structure incentivizes them to change carriers every few years, which disrupts the system for carriers and employers.
Let’s walk through how things got this way, why it’s an issue for everyone, and how BeneRe is approaching things differently.
How did voluntary benefits emerge?
Voluntary benefits were introduced decades ago, before benefits administration and enrollment systems came on the scene. These benefits include Accident coverage, Critical Illness coverage, and Hospital Indemnity coverage. They were created for the underinsured and uninsured in the early stages — basically, people who couldn’t get or afford health insurance.
Tens of thousands of salespeople were needed to enroll employees in these programs, and face-to-face sales with lots of paper-based transactions were inefficient and expensive.
To cover those high costs, heaped commissions were born. These are high first-year commissions, as high as 75%, which then trail to 5% to 15% annually after that. In addition, it began as a multi-level marketing structure where you could recruit people under your umbrella, and everybody would get paid at each level. Heaped commissions are also referred to as “high-low commissions,” since most of the commission is stacked up front.
This structure is very expensive and inefficient, but it grew the market substantially. Then, in the late 1990s and early 2000s, traditional employer-based private sector healthcare inflation significantly outpaced the consumer price index.
All of this has put lots of pressure on employer budgets for employee benefits. To combat higher costs, many organizations had to shift risk to employees in the form of high deductibles. Today, the average single deductible in America is $1,763, according to the Kaiser Family Foundation. Consider that number alongside the fact that according to a 2023 Bankrate survey, 57% of Americans do not have enough money to cover a $1,000 emergency expense. These emergency hardships are commonly healthcare-related.
For today’s traditional employers, voluntary benefits programs have become a way to offer a safety net for employees to cover the financial risk that was transferred to them due to higher deductibles and high out-of-pocket expenses. In addition, technology has emerged to create more efficient education and enrollment. Large employers have sophisticated benefits administration platforms that include consultative models and more employee education.
Unfortunately, the heaped commission structure still exists, even with these changes. These compensation structures do not mean that voluntary benefits specialists, consulting houses, or brokers are bad people – they’re just improperly incentivized. There is major misalignment to do what is best for their client when they are staring down a 75% year-one commission. This causes issues in several ways:
- The HR team and employees experience disruption from moving carriers
- There isn’t a value proposition improvement for employees
- First-year carrier losses lead to significant profits in subsequent years
- Employers don’t always know this is happening
In essence, insurance carriers see high short-term losses because of these large commission payouts that they then need to make up for by turning higher profits in the years following.
An example of a heaped commission problem
Let’s look at an example: Say ABC company has $1 million in total premium among their accident, critical illness, and hospital indemnity programs. If the carrier pays out commissions of 75% in that first year ($750,000), and then claims run 40%, that’s a huge loss before any other expenses of running an insurance company and paying internal teams. That drives a 35% loss in the first year, though claims don’t always run as high as 40%, which is a topic for another day.
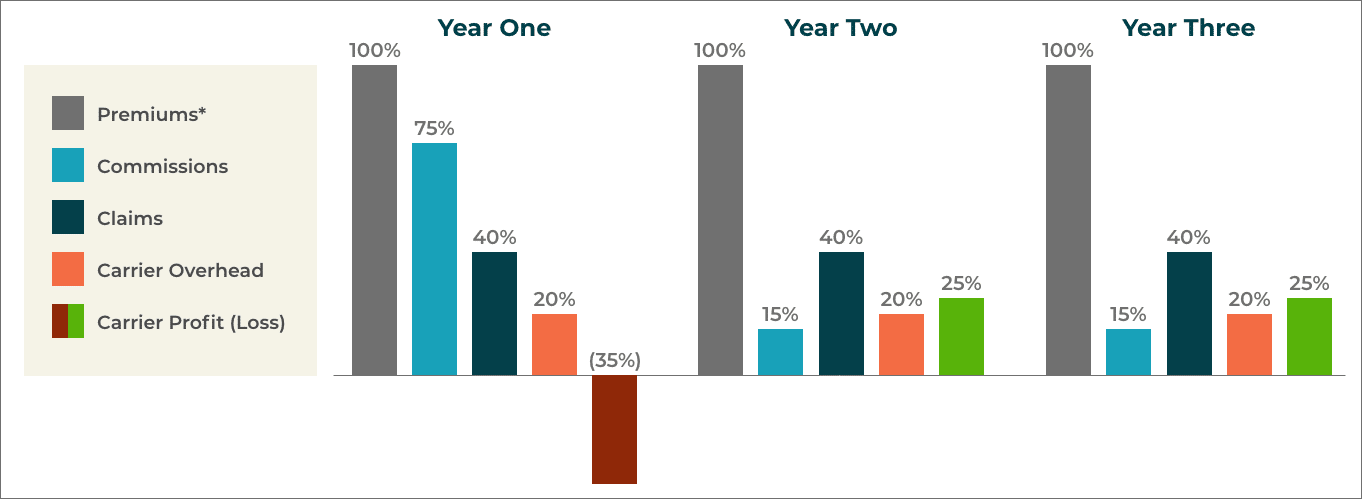
After the large loss in the first year, the carrier makes 25% in the second and third years in this example. Within three years, the carrier will get back to a profit margin in the cumulative sense of 5%. But because the claims often run lower than 40%, carriers are still very profitable even with this model.
Unfortunately, because of this corrupted business model, there is an automatic incentive in the industry to dampen the claims amount. This is an exhausting cycle for carriers. It’s as if they are renting customers for a few years at a lower margin, and they’d much rather see a level compensation structure.
What comes next?
The market is starting to catch on. Employers are gaining awareness and demanding transparency in payment structures. Still, many employers just don’t understand how heaped commissions work.
Often with voluntary benefits, commission reporting isn’t public information like it would be for other lines of coverage. That means these 75% commission amounts aren’t being disclosed most of the time, and that means HR departments often aren’t aware of it. Remember, these coverages are employee-paid, so they do not show up on the CFO’s budget — out of sight out of mind.
One answer to this issue is transparency. Everything should be reported in Form 5500, the Annual Return/Report of Employee Benefit Plan form, if the broker makes over $1,000 in a commission or fee. This isn’t always closely watched, however. This is why working with the right voluntary benefits insurance program is a must for total financial transparency.
Why work with BeneRe?
It’s important for any employer to understand how these commissions work to avoid issues with their voluntary benefits policies. Heaped commissions could continue to cause disruptions to coverage since brokers have an incentive to switch carriers every so often to get those high first-year commissions. Again, these are bad programs – not bad people. It’s just a hangover from the days when massive compensation was needed to support a huge salesforce of face-to-face enrollers. Today, technology efficiently does the work, but the large compensation remains.
BeneRe takes a different approach. We’re in business to assist big employers with Accident coverage, Critical Illness coverage, and Hospital Indemnity coverage by offering complete transparency, richer benefits at a lower premium, and distributing all underwriting profits back to the participating members to reinvest in employee programs. We ensure that voluntary benefits are financed the right way, with efficiency and transparency. This is an employee-centric approach that educates employers about best practices in the industry.
Reach out to BeneRe to set up a complimentary financial analysis of in-force programs or plans for new coverage offerings.
